Viral Road Trip - How COVID-19 Travels Along the Nerves
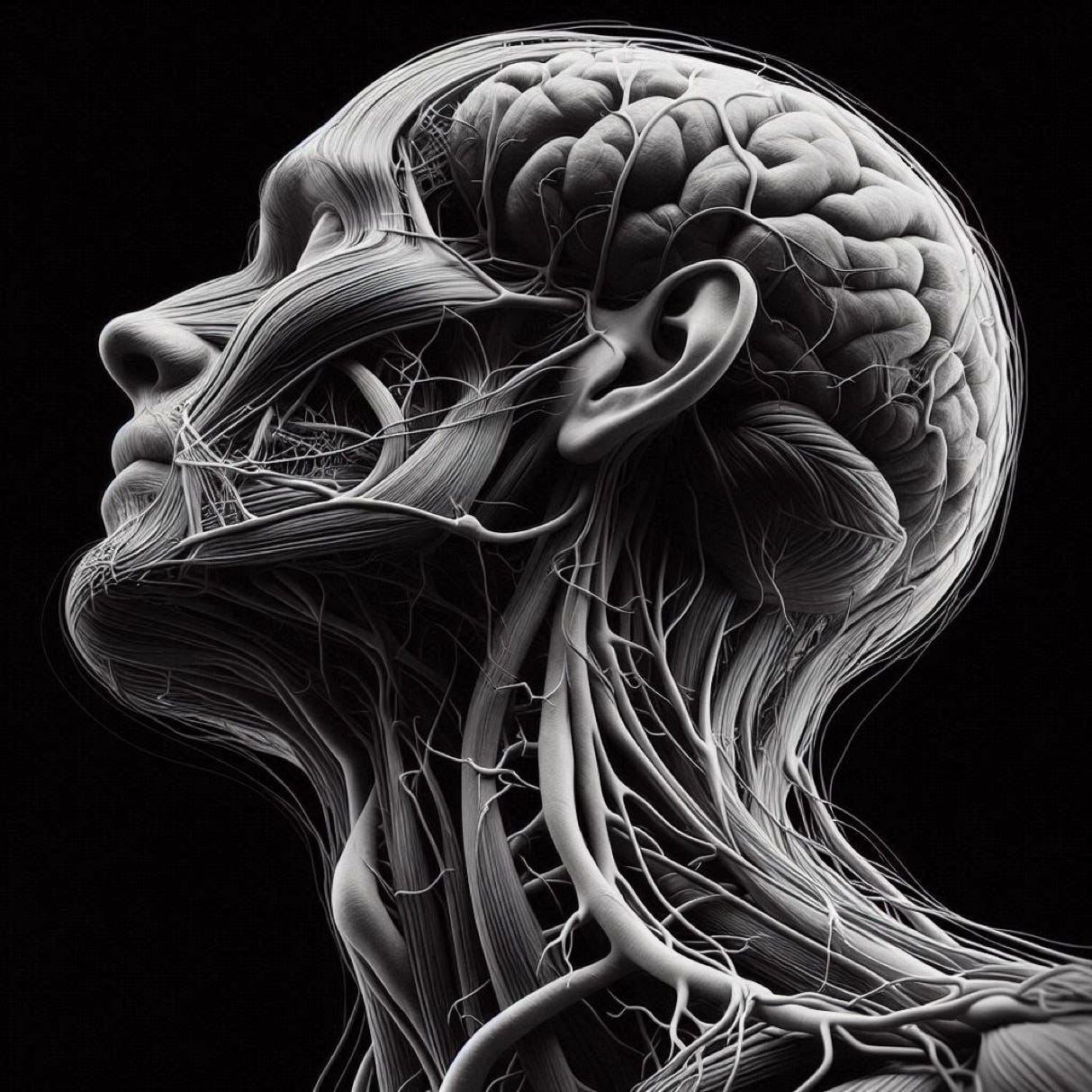
COVID-19 has shown that the virus can also affect the nervous system, leading to a range of neurological symptoms and complications.
One of the worrying aspects of SARS-CoV-2 is its ability to use the nerves like a highway to infect multiple areas of the body. This post explores the mechanisms by which COVID-19 can invade the nervous system and the implications of such neuroinvasion.
Mechanisms of Neuroinvasion
1. Direct Neural Pathways:
SARS-CoV-2 can enter the nervous system through direct pathways, such as the olfactory nerve. The olfactory nerve, responsible for the sense of smell, provides a direct route from the nasal cavity to the brain. The virus binds to ACE2 receptors, which are abundant in the olfactory epithelium and can travel along the olfactory nerve to reach the central nervous system (CNS)[2][5]. This route is supported by the presence of viral RNA in the cerebrospinal fluid and brain tissues of infected individuals.
2. Trans-Synaptic Spread:
Another proposed mechanism is the trans-synaptic spread, where the virus moves from one brain neuron to another neuron across brain synapses. This method allows SARS-CoV-2 to propagate through neural networks, potentially affecting various regions of the brain and peripheral nervous system[5]. This pathway is similar to how other neurotropic viruses, such as herpes simplex virus, spread within the nervous system.
3. Hematogenous Spread:
SARS-CoV-2 can also reach the nervous system via the bloodstream. The virus can cross the blood-brain barrier (BBB) either by infecting endothelial cells or by hitching a ride inside infected immune cells. Once across the BBB, the virus can infect brain cells and trigger inflammatory responses[2][4].
Neurological Manifestations
The neuroinvasion of SARS-CoV-2 can lead to a variety of neurological symptoms and conditions, including:
- Anosmia (Loss of Smell): One of the earliest and most common neurological symptoms, anosmia, is likely due to the virus's impact on the olfactory nerve[4].
- Headaches and Dizziness: These symptoms can result from the virus's direct effects on the brain or from systemic inflammation and blood clotting abnormalities[1][3].
- Encephalitis: Inflammation of the brain tissue can occur due to direct viral infection or as part of a broader inflammatory response[2].
- Cognitive Impairment: Many patients report "brain fog," memory loss, and other cognitive issues, which may be linked to direct viral damage or chronic inflammation in the brain[4].
- Movement Disorders: COVID-19 can affect motor coordination, leading to symptoms such as ataxia, tremors, and muscle weakness[1].
Long-Term Implications
The long-term neurological effects of COVID-19, often referred to as "Long COVID," can persist for months or even years after the initial infection. These long-term symptoms may include chronic headaches, cognitive deficits, and persistent anosmia[1][3]. Understanding the mechanisms of SARS-CoV-2 neuroinvasion is crucial for developing treatments and managing these long-term effects.
COVID-19’s capacity to travel along neural pathways shows the virus’s complexity, and it’s neurological impact. This understanding is crucial not only for managing acute cases but also for addressing the long-term care of patients suffering from persistent neurological symptoms.
Sources:
1. National Institute of Neurological Disorders and Stroke (NINDS) - COVID-19 and the Nervous System